Why Medical Practices Fail
Two weeks into my stint as acting CEO for a practice in which my consulting group had recommended the termination of the last chief executive, I was reviewing the previous day’s billing and collection activity when one of the physician shareholders walked in my office and placed an envelope on my desk.
As I picked up the envelope, he paused and simply stated, “That’s my resignation. I’m not exactly sure what my contract says, but this is what I want (relative to termination)…., as one of the founders of this practice, I don’t think that is unreasonable.”
As I started to explain that I would never expect him to be unreasonable, but his signed agreement was all that really mattered to me, he interrupted to say, “You don’t understand, I don’t care what my contract says; this is what I expect, period.”
Needless, to say, the remaining partners did care what his contract stated. However, that isn’t really the story. The story is why he resigned, and why, subsequently, an avalanche of resignations followed, and why a once thriving multi-specialty practice dissolved. Although you may not consider a physician practice in the same league or context as UPS, United or other employee owned Fortune 100 firms, the essence of an employee (physician) owned corporation is similar, and the rules for success are identical.
Quoting The Worker-Ownership Institute, “The keys to creating successful, democratic employee-owned businesses include the structure of ownership of the firm, the structure of worker participation in decision making, and the provision of training so employees can take an informed role as owners. Their consequence is the creation of a culture of ownership in firms in which ordinary workers know they are owners, benefit from ownership, are informed like owners, have opportunities for input, and consequently, act like owners.”
Usually, as is implied from the above statement, employees find it easier to act like employees than to act like owners. That’s because they start off as employees and become owners. The opposite is usually true in a medical practice, physicians start off as owners, creators, builders of a practice, and then find themselves employees. Their problem is learning how to act as employees, and when to wear which hat.
Most physicians are comfortable giving orders. Most are not as comfortable accepting them. However, the often critical missing element in group practices of small to medium size is an organizational hierarchy that correctly assigns responsibility and authority. To revisit the Worker-Owner Institute’s “keys,” “The keys to creating successful, democratic employee-owned businesses include the structure of ownership of the firm, the structure of worker participation in decision making, and the provision of training so employees can take an informed role as owners…”
By democratic business, we can take that simply to mean that shareholders have a voice. First, while structure of ownership is important, and can be used to either pull physician owners together or to encourage them to create individual fiefdoms, this isn’t intended to be a legal brief, so your ownership model will be assumed appropriate. However, you may simply ask yourselves if your ownership model is more supportive of the practice or of the individual shareholders.
The “keys” to focus on are “the structure of worker (i.e. physician shareholder)
participation and decision making and the provision of training” for “an informed role.” The physician I first described didn’t believe a structure existed for him to participate in decision making, and no training had occurred for him to become informed about his role as one shareholder among many. In this practice, the shareholders and the practice non-physician CEO met weekly to review practice performance and to discuss problems and issues. The practice CEO only attended part of the meeting, and was then dismissed. Trust was not high.
In this environment shareholders were not acting as shareholders or even as an executive board. They were acting as department directors and making employee-level decisions. In these meetings everything was discussed from bonus payouts to the how many times the phone rang before rolling over to the automated system. For these physicians, the meetings were frustrating. They believed nothing would, or should, happen in the practice unless they made the decision.
What could have saved this practice? First, the physicians had to want to save it. Second, the financial and operational problems of the practice had to be understood and corrected (which was my original consulting assignment). I had just spent two months doing that. They were on the road to economic and organizational correction. The last step was governance reorganization. This step never occurred.
However, had the physicians wanted to save the practice, these are the steps they could have taken.
First, the physicians needed to learn and understand their own organizational needs, skills and interests. Physicians in this practice took over operational duties because they felt out of control, didn’t receive good information, feedback or data from their staff and they were afraid of the consequences of the news they did receive.
This first step can be accomplished by beginning with categorical list building by each shareholder. What are their worries or fears, in what areas do they have a genuine interest in being involved, and what real non-clinical skills do they bring to the table. And, most importantly, what are their short and long(er) term career and personal goals. As this mostly subjective data is assembled, and it can be done in as little as an hour interview with each physician, the physicians should also take an objective career assessment. We use the Birkman Method®. Such an assessment serves as the “x-ray, EKG and SMAC 24” against which the subjective information is compared and validated. Once both subjective and objective data are gathered for each physician, an organizational diagram, or assessment, of the practice, with each physician plugged into his/her appropriate place can be created. This diagram defines the administrative roles of the physicians, the organizational needs they have and the necessary methods or processes to have those needs met. This analysis is the foundation for all further practice change and the development of the practice plan.
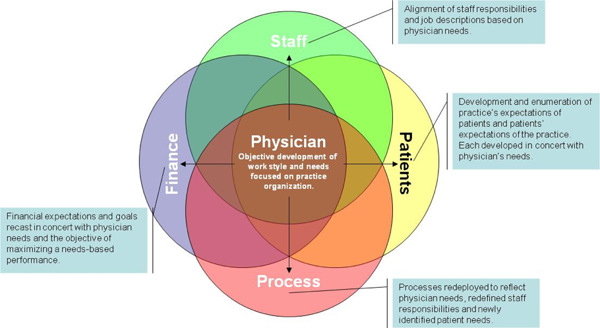
From that point forward, decisions concerning staff and their responsibilities, organizational processes and procedures, patient management and relations and financial decisions all flow from the initial analysis of physicians’ needs and personal goals and objectives.
Look at the Physician Centered Practice graphical presentation
The physicians are the “center” of the practice in my model. What is implicit is that the success of all other relationships or processes in the practice is contingent on the happiness, satisfaction and positive perspective of the physicians.
In this practice the physicians had lost sight of the big picture and felt compelled to focus on the most minor of problems and issues. However, each new problem was addressed in isolation rather than in the larger context of overall practice goals which derive from the collectivization of individual physician’s needs.
One final thought, when we speak of or advocate for physician-centered practices, a common retort is, “but we believe in a patient centered practice. Does “physician-centered” conflict with the currently popular “patient centered” practice? Absolutely not. In fact, we would assert that attempting to focus on the patient without addressing physician needs will result in very unhappy patients. By first defining and then developing strategies and processes to meet physician needs, patients, as well as staff, will be eminently more satisfied and happy. Communications at all levels will be improved, expectations will become clearer, processes will be better defined, and the practice will be more successful. And in the group practices, recognizing the importance of the shareholders’ relationships and needs are the beginning points.